Mohs surgery is a technique for the microscopically- controlled excision of skin cancer, producing the highest cure rate for non-melanoma skin cancers suitable for the procedure. The technique combines surgical removal of the skin cancer in a precise layer-by layer removal, with immediate microscopic examination of the removed tissue, using horizontal frozen sections to ensure no tumour remains.
Once clearance is achieved, the wound can be repaired. This process should not be confused with frozen sections, which refers to random, intermittent sectioning, examining only a small area of the overall specimen. Skin cancer is by far the most common malignant tumour in humans. The most common types of skin cancer are basal cell carcinoma, squamous cell carcinoma and melanoma.

Both basal cell carcinoma and squamous cell carcinoma begin as a single point in the upper layers of the skin and slowly enlarge, both along the surface and downward. These extensions cannot always be seen directly. The tumour often extends far beyond what is visible on the surface of the skin. Basal cell carcinoma metastasis (spread) is extremely rare, and usually only occurs in the setting of long-standing, large tumours. Squamous cell carcinoma is slightly more dangerous and patients must be observed for any spread of the tumour. Such spread is still infrequent. Patients with basal cell, squamous cell carcinoma and certain rare neoplasms should ideally be treated by this technique if they fall within one of the following criteria:

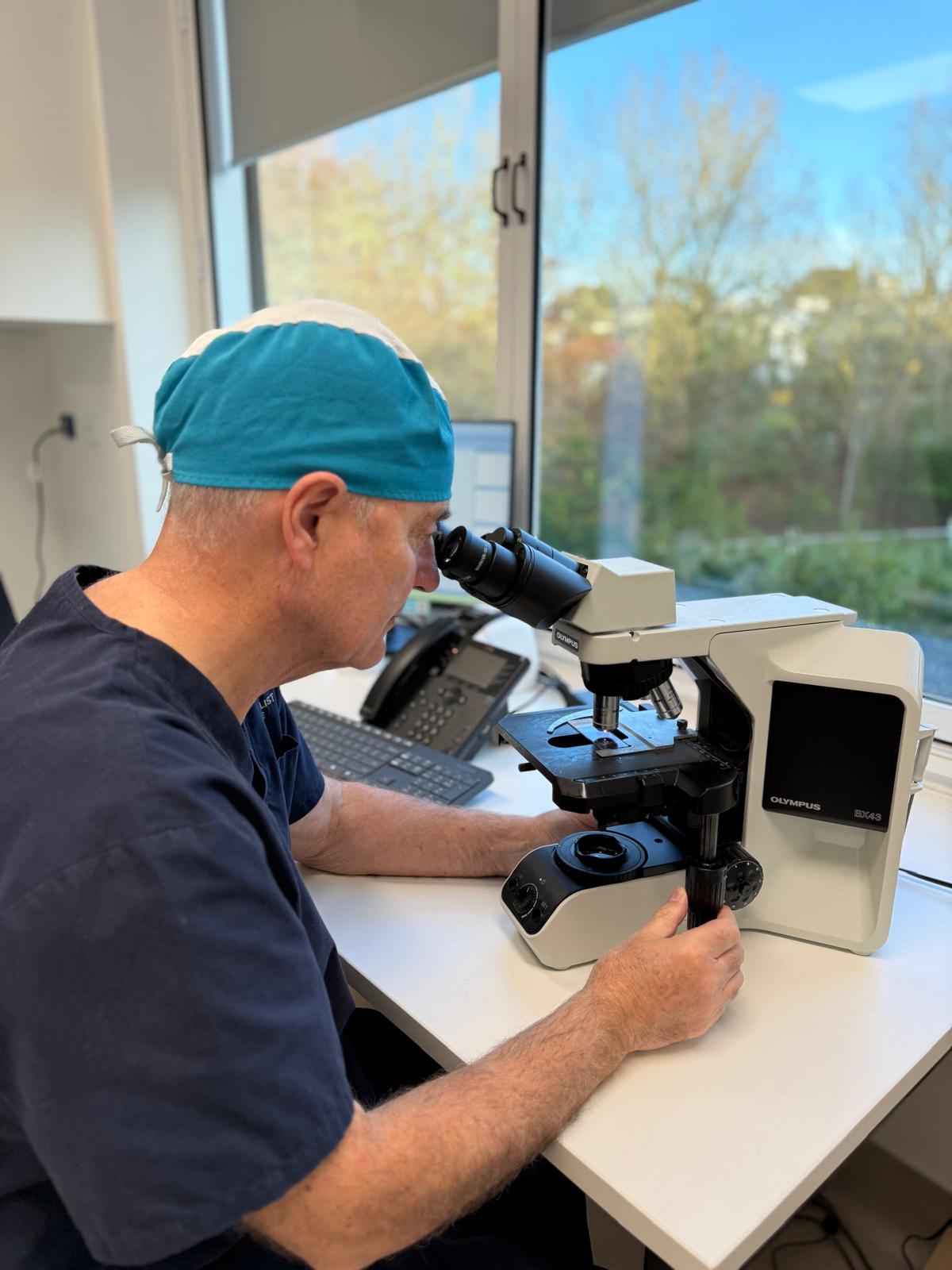
Dr Kevin McKerrow is a Mohs Micrographic Surgeon who completed a fellowship in Mohs Micrographic Surgery at the New England Medical Centre, Boston, Massachusetts in 1989 and established the first Mohs surgical uni in New Zealand.
He is a Fellow of the American College of Mohs Surgeons.
Clinical studies have demonstrated that Mohs micrographic surgery offers a cure rate of up to 99% for basal cell carcinomas and 97% for squamous cell carcinomas over a 10-year period.
Contact Us
Mohs surgery is a technique for the microscopically-controlled excision of skin cancer, producing the highest cure rate for non-melanoma skin cancers suitable for the procedure. The technique combines surgical removal of the skin cancer in a precise layer-by-layer removal, with immediate microscopic examination of the removed tissue, using horizontal frozen sections to ensure no tumour remains. Once clearance is achieved the wound can be repaired. The process should not be confused with frozen sections, which refer to random, intermittent sections examining only a small area of the overall specimen.

Mohs surgery is not required for treating all skin cancers. At Scars & Lasers, we reserve its use for cancers on the face and neck, where other treatment methods are often less effective.
Skin cancers in these areas are more likely to be inadequately treated with common approaches such as cryosurgery (freezing treatment), curettage and electrodesiccation (scraping and burning), simple excision, Imiquimod (Aldara cream), photodynamic therapy (PDT), or radiation therapy. Additionally, face and neck tumors are often more biologically aggressive and have a higher risk of incomplete excision with standard surgery.
Many skin cancers have invisible extensions or “roots” beneath the surface, especially if they have been previously treated. On the face, surgeons are often hesitant to remove excess healthy-looking skin to ensure complete cancer removal, as this can lead to both functional and cosmetic concerns. Typically, standard skin cancer surgery requires margins of 4-25mm of surrounding healthy skin to achieve a 95% success rate. While this is usually feasible for skin cancers on other parts of the body, removing even an extra 3mm of tissue on the eyelids, nose, or lips can have significant consequences.
Mohs surgery overcomes this challenge by precisely tracking and removing cancerous roots while preserving as much healthy tissue as possible. This results in higher cure rates and minimal scarring.

Not all facial and neck tumors require Mohs surgery, but it is particularly beneficial for tumors that:
By selectively using Mohs surgery for these cases, we maximize treatment success while preserving both function and appearance.


Patients should plan to spend the entire morning or afternoon at our centre on the day of Mohs surgery. The majority of skin cancers are removed on the first stage, however multiple stages are sometimes required. Each stage of the procedure takes around 30 – 45 minutes, the majority of which time is needed for our on-site laboratory to process the tissue so that it can be examined under the microscope.

You will be asked to return to Scars & Lasers for removal of your sutures following the surgery. It is also important that you receive regular skin checks with your dermatologist after the procedure to monitor for potential future skin cancers. The frequency of monitoring will depend on your overall skin cancer risk.
For all appointment enquiries, medical referrals and urgent enquiries please contact us at info@scarsandlasers.co.nz or (09) 524 5011.
